If you hear a creaking sound of the knee joint during exercise, this is the first sign of knee joint disease. Conservative methods of traditional and alternative medicine will help prevent cartilage destruction and maintain normal motor function. Treatment should begin immediately - only in this case will the rheumatologist give a good prognosis.
What is Arthropathy?
A non-inflammatory degenerative dystrophic disease that affects the largest joint (knee) is called knee arthropathy. A rather unusual medical definition, with a simpler "folk" concept - "salt deposition". Although the clinical manifestations of joint arthropathy are not related to excessive calcification of the knee joint. They have no effect on pathology and are a side effect of impaired metabolism.
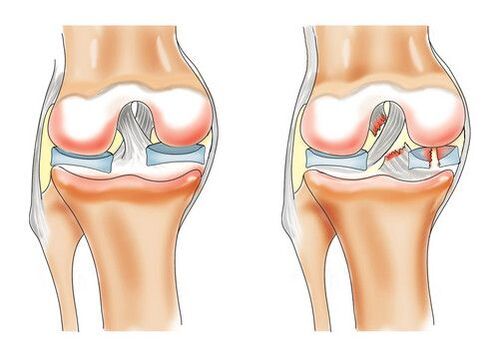
Negative processes in the hyaline cartilage contribute to the development of arthropathy of the knee, mainly poor circulation in the blood vessels of the small bones. The lack of nutrients and oxygen carried by lymph flow can lead to the breakdown of the outer layer of cartilage in the knee joint.
In its early stages, the disease is extremely difficult to identify. Joint deformity occurs slowly until the vitreous hyaline cartilage is pulled into the process. The anatomy of the ligaments was modified. Turbidity appears, the tissue thickens, thins, and cracks in all directions. The result of the pathology may be the complete loss of cartilage, which leads to tumors on the bone tissue and irreversible bending of the knee.
Disease classification
The International Classification of Diseases divides knee diseases into seven distinct subheadings:
- Bilateral primary knee joint disease. Diagnosis is most common in women 70 to 74 years old and men 60 to 64 years old. This puts the disease in the category of "older people".
- Another primary knee disease. A pathology of the knee joint due to natural wear and tear or the background of other diseases.
- Bilateral posttraumatic knee arthropathy. People of all ages with serious leg injuries are affected.
- Other post-traumatic arthropathy. Unilaterally, against the background of limb injuries and bruises.
- Other secondary arthropathy is bilateral. They are the result of chronic, incompletely healed bruises, fractures, or dislocations. It is most often diagnosed in athletes who carry weight on their legs - football players, athletes, figure skaters.
- Other secondary arthropathy. Unilateral development of pathology related to the specialty. For example, miners, metallurgists, fishermen.
- Knee joint disease, unspecified. It was diagnosed with an unexplained disease etiology after age, occupation, and genetic predisposition were excluded.
According to medical statistics, more than 10 million people of different age groups suffer from one or another knee disease. About 3, 000 diagnosed patients die each year.
reason
Knee osteoarthritis develops when cartilage loses flexibility and elasticity due to impaired metabolism of the knee joint.
Destructive processes are caused by a variety of reasons:
- Thyroid disorders against a hormonal background;
- Decreased vascular patency in the knee joint;
- genetic conditions;
- natural aging;
- past or present knee injuries, various sources;
- Obesity (over 20% of the norm), which puts a lot of pressure on the knee joint;
- Inflammatory arthropathy (polyarthritis, septic arthropathy);
- autoimmune disease (rheumatoid arthritis);
- Certain infectious diseases (syphilis, tuberculosis, encephalitis);
- Living in ecologically disadvantaged areas with poor food and water quality.
In addition, rheumatologists have identified several other causes that contribute to the development of knee joint disease. Neonatal stunting. With this diagnosis, joints wear out faster. Changes in collagen structure result in the destruction of proteins located in connective tissue.
Symptoms depend on the degree of joint disease
The initial stages of knee disease can be difficult to diagnose. Only the patient's own description of symptoms and external examination by a rheumatologist can draw a clinical picture of the progression of arthropathy of varying degrees:
- Degree I joint disease.Knee pulling pain, feeling a little stiff, partial loss of feeling, difficulty bending the leg, especially after prolonged immobility, inability to walk or run for a long time, slight swelling. Usually, symptoms go away with rest or simple anesthesia.
- Degree II arthropathy.At this stage, the pathology can already be determined by X-ray examination. The pain gets stronger and occurs after each physical activity. Discomfort can still be relieved by resting. Straightening your legs in the morning becomes more difficult and takes some time to regain motor function. Calf cramps are frequent, especially at night, which exacerbates the discomfort. During the movement, a crunching sound will be heard. Knee swelling is evident. There are obvious signs of limb deformity.
- Degree III arthropathy.There are irreversible changes in the knee joint. Cartilage abnormalities can be clearly identified on X-rays. The pain in the knee becomes persistent and severe. The leg stops bending at the knee. The patient was unable to walk without crutches or crutches. Swelling is noticeable. The anatomical shape of the knee is smoothed and given a solid appearance. The spine has primary curvature.

diagnosis
In order to make a correct diagnosis, it is necessary to combine the clinical manifestations of knee arthropathy with the patient's chief complaint. To clarify or rule out the cause of the disease, research is conducted in various ways.
The standard diagnosis is as follows:
- Make medical records of illnesses. Concomitant medical history, genetic predisposition, past trauma and surgical interventions, professional activities, etc.
- External assessment of deformation of the musculoskeletal system. Gait, posture, knee joint status, leg flexion.
- ordinary inspection. Palpate the lower legs, thighs, and damaged joints to localize the disease.
- lab testing. A general blood test provides data on the absence of an inflammatory process. If this process is present in the context of other diseases, the erythrocyte sedimentation rate in the blood increases. Levels of protein, globulin, and fibrinogen will vary from normative targets. Biochemical components will remain within standard ranges. Knee synovial fluid biopsy is performed if pathological progression is at an advanced stage.
- Instrumental Research. X-rays are the main and most common method for diagnosing suspected knee arthropathy. Often, rheumatologists can easily identify changes in bone tissue structure from pictures at the beginning of stage 2 of the disease. With the help of more modern and accurate equipment - MRI, CT, ultrasound, bone scintigraphy, thermography to diagnose the presence of secondary diseases and their causes.

treat arthritis
Like all joint disorders, knee joint disease requires systemic treatment, which is best started when the first symptoms appear. In this case, the prognosis of the treatment becomes favorable and a return to a normal lifestyle is guaranteed within a fairly short period of time.
Comprehensive treatment aims to eliminate the main signs of the disease:
- discomfort, pain syndrome and muscle tone;
- Improve the motor function of the knee joint;
- stop the process of cartilage destruction;
- strengthen connective muscles;
- Restore normal blood circulation to the knee joint.
drug
Anti-inflammatory drugs
They help relieve pain and relieve swelling caused by inflammation of the muscle tissue.
chondroprotective agent
Without chondroprotective agents, regeneration and recovery of cartilage tissue is impossible. They are a major component of conservative treatment.
vasodilator
They are used to improve the patency of blood vessels in the joints.
hormone drugs
Reduces production of the hormone cortisone to prevent the development of inflammatory processes.
Hyaluronic acid injection
Used to restore intra-articular synovial fluid. As a result, friction between joint sites is reduced, motor functions are normalized, and the elasticity of cartilage tissue is restored.
anti-enzyme
They inhibit the activity of trypsin, thereby preventing further damage to the joints. Appointment in the complex.
physiotherapy
Physiological therapy has been used successfully to treat knee osteoarthritis for decades. It can be used as a separate type of treatment during prevention or recovery. The same goes for an integrative approach to the disease.
In most cases, a rheumatologist will prescribe the following types of procedures:
- Painkillers electrophoresis;
- ultrasound therapy;
- magnetic therapy;
- laser exposure;
- Paraffin application;
- mud treatment;
- therapeutic exercise (exercise therapy);
- Manual therapy, massage with ointment.
Surgery and Prosthetics
If the knee joint disease is in an advanced stage and the knee joint and cartilage tissue are destroyed, it is not possible without surgery. Otherwise, the person will be disabled for life.
Modern medicine offers several solutions to the problem:
- Arthrodesis. The affected tissue and knee joint are completely removed. The body is liberated from the lesion, but the motor function of the limb is completely lost. It is rarely used if the patient has other joint disorders.
- Arthroscopy. Destroyed hyaline cartilage is removed. The surgical trauma is small and the recovery period is short. It is suitable for patients whose progression has not affected the knee itself.
- Periarticular osteotomy. A complex operation, the essence of which is to archive deformed bones and growths and then attach them to the necessary anatomy.
- Built-in prosthesis. The completely destroyed knee joint was removed and a titanium prosthesis was placed in its place. An effective way to make you forget about knee disease forever. Careful preparation and long-term rehabilitation are required.
traditional medicine
The use of folk remedies and conservative treatment can relieve external symptoms (pain, swelling). Recipes based on bay leaf, burdock root, St. John's wort, malt and hay have proven themselves well. Ointments, creams, tinctures, and decoctions are made from them.
These plants have anti-inflammatory and analgesic properties. Regular and long-term use is required to achieve visible results.
Honey-based ointments and compresses, along with alcohol or apple cider vinegar, are great for relieving swelling and calming the affected tissue.
The nutritional blend is made with lemon and garlic and is taken by mouth with one teaspoon each after breakfast and dinner. Such recipes have a general strengthening effect on the body, increasing the patency of blood vessels and nourishing the joints with useful trace elements.
It should be remembered that home treatment does not eliminate the main problem - pathological destruction of the knee joint.

diet
Adherence to the diet is an integral part of complex treatment. Adjusting your diet not only helps with weight control, but also provides essential vitamins for your bones and joints.
In patients diagnosed with arthropathy, contraindications:
- Fried, spicy, salty, pickled food;
- fat soup;
- sweet pastries;
- Fruits, high in acid enzymes;
- Alcoholic beverages.
Menus should be supplemented with raw vegetables, fruits and herbs, low-fat yogurt products, bone broth, and dishes containing gelatin (jelly, jellies).
Other methods
For the treatment of arthropathy, it is necessary to have regular hydrotherapy, at least once a year, and more frequently if possible. The procedures of hydrotherapy, mud therapy and manual therapy can preserve the disease for a long time and prevent the destruction of the joints.
It will take the rest of your life to maintain your sore knee in a stable condition. But it can be very useful for the whole body. Review nutrition, eliminate bad habits, exercise, visit resorts - quality of life can be significantly improved.
It should be remembered that self-medication, ignoring the main symptoms and the unbearable stress of a sore knee can quickly turn a healthy person into a helpless disabled person.






























